The human heart is a remarkable organ, tirelessly pumping blood to sustain life. Central to its function are the four heart valves, which ensure unidirectional blood flow through the heart’s chambers. Among these valves, the mitral valve holds special significance as it regulates blood flow between the left atrium and the left ventricle. However, at times, this valve can become compromised, leading to a condition known as mitral valve prolapse (MVP). In this article, we will delve into the intricacies of mitral valve prolapse, exploring its symptoms, causes, diagnosis, and available treatments.
Understanding Mitral Valve Prolapse:
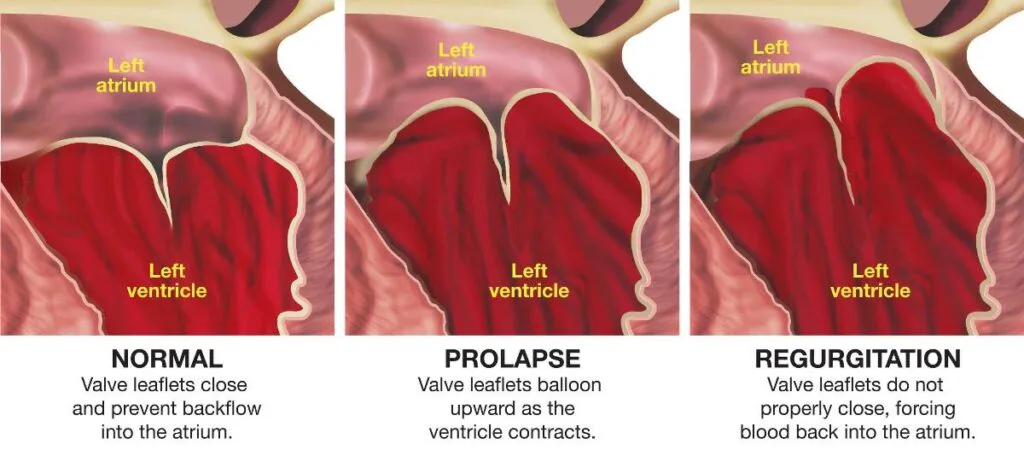
Mitral valve prolapse occurs when the valve’s flaps do not close properly during the heartbeat, allowing a small portion of blood to leak backward into the left atrium. This condition is relatively common, affecting about 2-3% of the population, with a slightly higher prevalence in women. MVP often goes unnoticed, and many individuals with the condition lead normal, healthy lives without experiencing symptoms.
Symptoms:
While many people with MVP remain asymptomatic, others may experience a range of mild to severe symptoms, including:

- Heart Palpitations: Individuals may feel a sensation of rapid, fluttering, or irregular heartbeats.
- Chest Discomfort: Some individuals may experience chest pain or discomfort, often described as sharp and fleeting.
- Fatigue: Unexplained fatigue and a decrease in energy levels are commonly reported symptoms.
- Shortness of Breath: Difficulty breathing, especially during physical activity or when lying flat, can be indicative of MVP.
- Dizziness or Lightheadedness: These symptoms may result from irregular heartbeats or decreased blood flow.
Causes:
The exact cause of mitral valve prolapse is not always clear, but several factors contribute to its development:
- Genetics: Family history plays a significant role, with a genetic predisposition to MVP observed in some cases.
- Connective Tissue Disorders: Conditions such as Marfan syndrome and Ehlers-Danlos syndrome, which affect connective tissues, can increase the risk of MVP.
- Structural Abnormalities: Individuals with certain structural abnormalities of the heart may be more prone to mitral valve prolapse.
Diagnosis:
Diagnosing MVP involves a combination of medical history review, physical examination, and diagnostic tests. Doctors often use a stethoscope to listen for a heart murmur, which can indicate abnormal blood flow. Echocardiography, particularly a transesophageal echocardiogram (TEE), provides detailed images of the heart’s structure and function, allowing healthcare professionals to accurately diagnose MVP and assess its severity.
Treatment:
Treatment for mitral valve prolapse varies based on the severity of the condition and the presence of symptoms:

- Lifestyle Modifications: In many cases, individuals with MVP can manage their symptoms through lifestyle changes such as reducing caffeine intake, managing stress, and engaging in regular physical activity.
- Medications: Beta-blockers and other medications may be prescribed to control palpitations, chest pain, and other symptoms.
- Surgery: Severe cases of MVP that lead to significant valve leakage or other complications may require surgical intervention. Minimally invasive procedures or traditional open-heart surgery can be used to repair or replace the mitral valve.
- Regular Monitoring: People with MVP should undergo regular medical check-ups to monitor their condition and assess any changes.
Conclusion:
Mitral valve prolapse is a common heart valve disorder that, for many, poses no significant health risks. Understanding the symptoms, causes, and potential treatments for MVP empowers individuals to take control of their heart health. If you suspect you might have MVP or are experiencing any cardiac symptoms, seeking medical evaluation and guidance is essential for accurate diagnosis and appropriate management.